No specialty has been more affected (compromised?) by the notion of work hour reform than general surgery. With the introduction of the 80 hour work week, surgical interns and junior residents saw their hospital contact time cut drastically with deleterious consequences in terms of case load and relative comfort level taking care of typical surgical complications. Other data suggests that errors are paradoxically increased when surgical residents are forced to go home early post call because of continuity of care issues during patient hand offs.
I know I sound like a crotchety old timer, longing for the days of stumbling into my tiny studio apartment in Chicago as an intern with the AC broken, mindlessly whipping up a pan of Kraft mac and cheese, eating directly from pan, and crashing out on the couch with the half eaten mac/cheese on the floor and the TV on and the alarm set to go off at 4:00Am the next morning. Such fond memories indeed. But that sort of regimen made me an anal, relentless, rarely satisfied, tireless surgeon (at least when it comes to patient care). And everyone went through the same thing. So we held each other accountable. It became a way of life (goodbye golf, having beers till 2Am on a random Wednesday in Lincoln Park). And I don't regret it for a minute. I was brainwashed and indoctrinated, most definitely. But I wouldn't be the surgeon I am today without the experience of old school residency. You just can't make up for the lost face time and hours and hours of hours of unfiltered hospital life. There are no books you can read at home to reproduce it. No Youtube videos to watch. No "intensive resident education seminars" that will replace the value of simply spending an ungodly amount of time in the hospital.
One of the arguments for work hour reform is this idea that residents spend too much time doing scut. Scut is the bane of the intern's existence. Go draw a CBC on patient X. Go wheel Mr Y down to cardiology for his stat echocardiogram. Go down to radiology and get hard copies of Mrs M's MRI. Write transfer orders on 6 patients in the ICU. Call the outside hospital to get records of patient G faxed to us by noon. When the senior residents would alight their gaze upon you with that look of "Man, I hate to have to ask you this but..." it's just soul crushing. But you did it. The whole time you're grumbling to yourself about how such mindless toil is beneath you and unworthy of the efforts of someone so highly educated. Is this why I studied so hard all these years?
But a funny thing happens when you spend so much time in the hospital. You find yourself seeing things and experiencing events that change you fundamentally. Little things like chatting with an elderly man while you wheel him down to CT scan, making small talk, learning about him as a human being, rather than simply a name on the list. Watching a veteran nurse in ICU handle a difficult family. Observing how difficult it can be for proud, independent men and women to be thrust into the role of dependent patient, institutionalized, helpless. Seeing the grimace on a patient's face when you're drawing his blood. And there's also the major events. The code blues that are called and you're the only physician around. The post op liver transplant in the ICU who's not doing so well and you end up sitting at her bedside all night, watching the monitors, reacting to the subtle real time alterations in her condition. The emergency colectomy that comes in while all the senior residents are busy doing other cases and you're the only one left to assist. The possibilities are endless. But you have to be present. You have to be in the hospital. The experience is yours, if youre willing to seize it.
You see, there's more to being a doctor/surgeon than just learning how to fix a hernia or run a code. There's a mindset that has to take hold. Call it indoctrination if you like but it's a process that attempts to transform a self-satisfied, smug, well-educated medical student (I certainly fell into that category) into the sort of selfless, compassionate, dedicated, thorough, and mindful physician that we all deserve (a gradual transformation that doesn't end just because you've become an Attending, believe me). The scut work and mindless b.s that junior residents used to have to endure has a lasting effect. One's immersion into the totality of hospital life as a trainee leaves a lifelong mark. Even today, I make my rounds the same way I did when I was an intern. I sit in front of the computer and dutifully write down all the vitals and lab results of my patients in little chicken scratch boxes. I review the xrays and medicine lists. I make up a preliminary plan. And then I go see everyone, one by one. It's very banal and systematic. Nothing's changed, only the degree of ultimate responsibility.
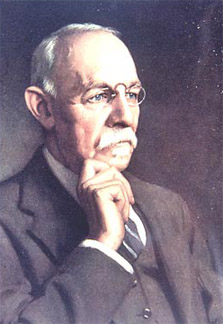
Imagine the military without basic training. Football without two a days in the July heat. Medical school without the grueling second year of no sunlight and 10 hour library sessions. A lot of guys can throw a nice tight spiral on the practice field, but that's not what makes a great quarterback. It's the guy who can make the clutch throws late in the game when he's exhausted, banged up, and all the pressure is on his shoulders. The kinds of people who can perform when the chips are down aren't always born that way. Mental toughness is malleable. And I think that's what Dr. Halsted had in mind when he pioneered the first surgical training program at Johns Hopkins....
21 comments:
Griffey-esq swing but still a miss. In my medical school experience, there is a direct coorelation between the number of nasty patient-dehumanizing residents and the extent of that program's hour violations. Maybe it's in the early hours of the morning when no medical students are around that humanism is born like a phoenix from the flames of crappy hours; but i doubt it.
Current estimations of the reduction in case-loads of graduating surgical residents is about 10~15%. Keep in mind a large majority of surgical residents now go for fellowships, and add another year or two of op-experience on top of that.
There has never been a change in any education system that the previous generation didn't lambast as the end of intellect and adequate training. You are suffering from the nostalgia and conservatism. We need scut about as much as we need ancient greek and latin taught in grade school. And Halstead was too busy doing cocaine under house-arrest to think much about scut, i'd blame Cushing.
Thanks for the memories Buckeye...
I loved chattin with that elderly guy too...except I was the one disimpacting him...
How about signing delinquent charts for the Intern who had to go back to Iran? Guy got drafted into the Army rather than do 2 more years of Infernal Medicine...
Frank
As usual, very well-written. But I can't help but hear this as another "in my day" line of thought. If I could take you back in time, make you relive your twenties, and then do surgical residency again under the 80hr work week, it would be the only way to actually be able to say 'then' was superior to 'now'. As one of the ones doing it now, I can identify with every sentiment you wrote about. It has to do with what kind of person you are and to what kind of standard you hold yourself. I have no doubt in my mind that 100-120 hr weeks produced plenty of terrible physicians in all specialties, and that there will be plenty of impassioned, dedicated, intelligent 80hr folks too.
Very nice, Buckeye.
The old guard has picked on duty hours as the reason for the change they perceive in us, but in truth it is multi-factorial. As a med student, I now am not allowed to have any responsibility. My notes didn't count. I was not allowed to even attempt a central line until the end of fourth year, if then.
Patient contact is decreased by the amount of time residents spend not drawing blood or talking to patients but filling out check-boxes and copying medication lists from the computer onto a form for the nurse to also copy. "Quality initiatives" must be satisfied, after all.
It may be true that we are not the physicians of old, but we do not practice in the same environment, either. Core skills are still learned in my speciality despite duty hour restrictions. If hand-offs increase error, that's because the hand-offs are done poorly, not because the resident who hasn't slept for 45 hours would've somehow done a better job.
Don't kid yourself that you were somehow perfect or even adequate after two or three days without sleep. It's just that no one was tracking your outcomes. The duty hour initiatives and quality improvement paperwork I'm saddled with came as a RESULT of the prior generation's practices, not as an a priori brainstorm from some office worker.
I've got a friend in ENT residency and he is worried about the hour limitation they get. Plenty of people at his program "sign out" but hang out at the hospital for a couple more hours. Everyone is trying to get in on the "cool" cases but with work restrictions you aren't around as much. Eventually they might have to tack on another year to surgery residency to make up for it.
This will be a bit off topic, but I think that the previous comments have generated appropriate debate. Therefore I would like to turn my attention towards Tyro's comment.
Tryo,
You're correct for but for the wrong reasons.
"Don't kid yourself that you were somehow perfect or even adequate after two or three days without sleep. It's just that no one was tracking your outcomes."
Our outcomes as surgeons are tracked better than any other specialty through the structured M&M process. This is the core of our training and is unique to surgeons. During residency we were directly responsible for each patient's outcome and stood in front of the department every week during M&M to explain why our patients had complications. Do you present all of your cases at the end of each week, and review your complications in a structured formal process?
"The duty hour initiatives and quality improvement paperwork I'm saddled with came as a RESULT of the prior generation's practices, not as an a priori brainstorm from some office worker."
I preface my comments below by first stating that I support improving resident training by creating a better working environment and reducing unnecessary, wasteful and/or abusive work hours. But let me correct you before you try to rewrite history.
Duty hour initiatives came from lawyers. There was no real thought process other than "residents worked too hard" and "this must be unsafe". There was no effort given to figure out what the appropriate duty hours would be. The 80 hour number quite literally was just picked because it sounded right to "some office worker".
The documentation that you are saddled with did not come as a RESULT of prior generation's practices. It came as a RESULT of a myriad of interconnecting issues associated with the remuneration of services provided. Documentation, as it stands now, has nothing to do with the practice of medicine. It has everything to do with the payment of services.
I have spent over decade trying to engage in improving electronic medical records. In so, I have found that the rules continue to change such that a greater burden is added on the providers to document more. This has not resulted in any tangible improvement in efficiency, communication, nor patient safety.
Documentation should be used as a tool to augment communication between providers of care such that they become more efficient (measured by improved performance), and patients get better care (measured by improved outcomes). This has yet to happen.
Now, that I have had my tirade I will end with this. Duty hour restrictions are not going away. Stop lamenting this; it serves no purpose. Our job is to redefine medical education. We must find better, more efficient processes by which to train our students so that they will be better physicians than we are today.
JFS
I agree, work hour reform is inevitable. What prompted this post was my dismay at discovering that it is universally assumed that all "scut" is useless, mind-numbing bs. Scut is basic training for an apprentice surgeon. Scut for a year or two makes you more efficient, more anal, and more thorough. I won't budge from that stance. If we have to add another year to residency or restructure residency such that those looking to do fellowships are shunted off into specialty tracks at an earlier stage of training, then so be it. But scut is not fundamentally the great evil that eveyone tries to make it out to be.
But it is in the scut that a physician begins to find themselves as well. Hard to believe, but we should all realize that tracking down patient data, wheeling them to the radiology suite late at night, putting in IVs and getting labs when others couldn't (or wouldn't) generates a personal work ethic. It is sometimes easier to just "wait and see" rather than actually do the task. It's easier to say that you asked the outside hospital to fax the pt's information and they didn't rather than actually doing it. But, if you do this, on top of a busy night with cross cover, admits, etc. it lends a certain credibility to your work.
There have been times where I've cut a corner or two and have been bothered by it for days or weeks. Fatigue can make scut seem pointless, but there is a purpose - usually.
Buckeye, as you know, I am not a medical student and cannot speak to what you all go through.
In my clinical experience, being a second career student, I do pass judgment. I can pick out the professionals with trench experience easily. I tend to feel a sense of calm if my patient's surgeon or internist has scut experience. More often than not, those who have both feet in this thing, will involve me, teach me as well. We work together not against each other. The fact that I am new at this is not a surprise, and not a problem. Some of those who are not "all in" tend to lay blame for their inadequacies on anything that moves. I have not been on the receiving end of that (yet). I do become anxious however working with this type because I do not have confidence in them, and subconsciously question their every move because they tend to act out of fear and I am protective of my patients, myself, and of other staff.
-SCNS
You chaps should feel lucky you are allowed to work 80 hours a week. Over here, in Europe the mindless EU has imposed a 48 hour limit. (the European Working Time Directive)
I have seen terrible physicians who still ramble on about how they were working 120 hours a week in the old days (1960-1980s). It does not sound enticing.
Unfotunately current leaders have gone overboard and made the medical profession akin to most office jobs.
There will definately be a drop in my surgical experience and ability. This will mean a longer training time.
But overall, the peristent obsession of my peers with subspecialisation will somewhat reduce the impact of the reduced training time. There is a gradual move towards reducing the variety of procedures performed by a general surgeon depending on the subspecialty chosen. Repetition of a reduced repertoire of surgical procedures will invariably lead to excellent surgical abilities alebeit in a very narrow field. Or to put it in a nutshell, it will all become "monkey business"
This is the real problem with the reduction in working hours. It simplifies, segmentalizes our profession and in many ways diminishes our subjective value.
I think the 80hours you got are pretty much spot on. 120 was overkill and most likely unsafe regardless of how tough you were.
You should hold on to what you have. Europe has gone completely in the wrong direction. I'm even thinking of trying out your 80 hour system for myself...
A couple points:
1: I trained before the 2003 rule change. All I have to say is good riddance. Some of the worst residents I every saw where the surgical residents working over there 100th hour. They were rude (to staff, other residents, patients, and family), impossible to get to the patients bedside, and at times incompetant due to sleeploss. In hindsight, I don't blame them, I blame the dehumanizing system.
2: Dear Joe, surgery is not special. Many residencies (including my own) have a formalized regular M&M process. Maybe you need to step outside the rarefied confines of the OR to see how the other half lives.
3: Dear Joe: The 80 hour work rule not picked out of some bureaucrat's ass at the RRC. It was based on New York State's experience. Jeez, look it up.
I had a discussion about this the other night.
On one side of the argument, there's the stipulation for a certain amount of time spent in the hospital, but what about the increase in error from tired physicians? If I remember correctly, a certain amount of sleeplessness stacks up to being somewhere near drunk. (Not that I know the precise amount, but being a neurobiology student, I've been educated on sleep and the brain)
Nostalgia doesn't solve problems, and I'd hate to be treated by someone who was in the last 20 hours of their 80-hour work week, because it's painfully obvious that they're closer to dragging ass than someone who's well-rested.
I respectfully but completely disagree with you. I've been in the trenches doing scut for the past 3 years of residency, at the large expense of more operating. How much time in my average week was I in the OR compared to on the floor doing uneducational work? It's literally 10 hours of operating out of 80. Sure, I've spent quality time with patients and been the only one around in code situations, but compassion comes from within and thrives in spite of, not because of, long excessively burdensome hours of scut work. That doesn't make you a more humanistic physician; it makes you bitter, angry, and resentful. This continued focus on service above all else instead of education continues to make surgery unattractive and in my opinion has a lot to do with the continued outrageously high (~20%) attrition rate from residency.
You know, I think I'll weigh in here with my.... unique perspective. You used the example of the military and basic training to justify scut in modern surgical training. I think I have a rather unique perspective here...
I graduated from infantry basic & advanced training in 1987. Since then I've spent my entire adult life in the military, and now I am a surgery resident.
When I went to basic, there were 2 locations on Ft. Benning where trainees were housed: Sand Hill and Harmony Church. Sand Hill had fairly modern barracks, and where I was, Harmony Church, had WW2-era "temporary" wooden buildings that probably should have been condemned. We had to buff the floors to a high shine, however, and spend hours on our hands & knees applying brasso and elbow grease to brass plumbing fixtures in the latrine - I kid you not. No, we did not use toothbrushes to clean the toilets like they do in the movies, but we did have nothing but hand-held rags and simple green, and if those toilets didn't SHINE we did push-ups until the cows came home...
We used to fantasize about the lucky guys in Sand Hill, who had air-conditioned barracks that were not falling apart at the seams, no exposed fixtures, and were easier to keep clean and presentable because bits of the ceiling weren't continually raining down upon their heads (I am not making this up).
We, graduates of Harmony Church, were convinced we were that much harder and better than our softy cousins from Sand Hill.
Six months after basic training, as still quite green infantryman in our first real units, do you really think any of us could tell the difference about where we had graduated from? And even more humorous was the complete indifference the experienced soldiers in out unit had to whether or not we could brasso a plumbing fixture. All they cared about was whether we were hard workers who wanted to learn and excel in a dangerous job where teamwork sometimes meant meant coming home alive.
It was the essential challenge of basic training that created infantryman out of civilians, not the details of whether they had to do extra work to spit-shine a plumbing fixture.
So please, wax nostalgically about your work as an over-educated discharge coordinator or social worker. The graybeards in your program no doubt waxed poetic about how much they learned while performing their own CBCs, or doing their own EKGs. The fact is, it isn't THOSE guys who are the ones telling me I'm missing out on training because I'm not wheeling patients to the CT scanner myself... it's the mid-level 40 -year olds. The graybeards have been around long enough to realize that much of what they were put through was worthless BS that only served to provide hospitals with cheap labor... just like after 22 years of military service I realize that passing through Harmony Church did not make me any better of a soldier than my (softy!) cousins going through Sand Hill.
Oh come now you aren't wheeling anybody anywhere nowdays unless the patient is crashing. It has gotten to the point where surgical residents are calling ICU/floor patient management "scut". God help us all when you actually get into the real world (reality check, the ivory tower where you actually haven't practiced medicine under your own independent license for one minute is NOT the real world). I would expect more from a fellow ex-military.
Late to the conversation, but I wanted to add my agreement as a surgical resident that a lot of what we call "scut" is an important way to learn to take care of patients thoroughly and efficiently. Yes, I hated starting rounds at 4am as an intern. But I learned how to gather essential information quickly, and how to deal with little morning emergencies quickly, so as not to lose time. I don't have quite as hard a job rounding now that I'm not an intern, but I know the habits I learned then will last for the rest of my life.
To the first anonymous: the reason everyone does fellowships is because we know we're not getting enough training under the new regime. If I had known coming in that I would have to spend 7-8 years, instead of 5, to be fully trained, that would have discouraged me more than the hard work ever did.
But Buckeye, are you sure some of it doesn't look rosier in retrospect?
Dr. Parks,
Where do you draw the line between patient safety and resident work hours? Personally, I would not want to be treated by a physician who has not slept in 24-36 hours. It seems to me the risk of making a mistake would significantly increase compared to a well rested doctor.
Another view:
http://www.dallasnews.com/sharedcontent/dws/news/localnews/stories/080110dnprosupervisionimpact.2903d42.html
Don't pull a muscle while your trying to pat your back there. :) Every surgeon out there thinks he/she is the world's best because of long residency hours. I think the 120 hr work week produced some good surgeons IN SPITE of the work hours, not because of them.
This is another post of "oh, the good old time". Any profession field track safety outcome can show that cognitive ability after extended period of sleep deprivation equals legally intoxicated. You might argue that surgeon trained themselves to be functional from those 80-120 hr/wk , but that amounts to saying drunk drivers adapt themselves to drive while intoxicated until the accident happens. I will challenge the author to take Q3 calls, and stay up 30 hours dealing with patient care on every call in current practice environment and manage the well being of himself, his family and his patients.
We are living in a very different health care environment now. From my own surgical residency training experience from this time, the amount of scut work is taking up increasingly more proportion of the valid hands on and direct patient care related activity. The problem is not the amount of hours, rather what percentage of time spending in learning activity during these 80 hrs. All the endless scut, as the author romanticized, doing the transporter's job etc.....are at the large expense of more time that should be better spend in education and training.
Post a Comment